The concept of telemedicine is not new. While there were many attempts to develop telemedicine programs in the 1960s, inadequate technology made this practice futile. While research and development of telemedicine started in the 1990s, it definitely took centre stage during the COVID-19 pandemic.
Regarded as the “natural evolution of healthcare in the digital world,” the development of digital technologies and the mandatory social distancing norms of the COVID-19 pandemic popularised telemedicine as the safest interactive system between patients and doctors. While telemedicine was capable of improving healthcare access for hard-to-reach populations, it also showed potential in bridging the communication gap with the help of language experts like medical interpreters and translators.
What is Telemedicine?
As the name suggests, telemedicine is the practice of using technology to deliver healthcare from a distance. In no time, it has taken an integral role in the modern healthcare system.
Telemedicine services typically use a computer, smartphone, tablet, or another mobile device, and they rely on secure video and audio connections. As for the types of services, there is a wide range, including:
- Consultations
- Medication management
- Chronic illness management
- Follow-ups and more..
A medicare expert in one location can use a telecommunications infrastructure to provide care to a patient at a distant site. It includes all appropriate tools and resources that assist clinicians in reaching and periodically monitoring individuals who have difficulties attending specialist visits, especially patients affected by chronic diseases who require continuous follow-up. These patients’ health can be assessed by sending the data recorded on the digital tool to a specialist. In addition, telemedicine also helps when two medical experts communicate virtually, for example, a general practitioner sending photographs or videos to a specialist for their opinion.
By developing such a digitalised setup, there is no need for patients to wait around in the lobby waiting for an appointment. Instead, they can get a doctor’s opinion without much hassle and expenses. This arrangement also helps hospitals decongest by determining which patients need urgent medical attention and which ones can stay at home and get better with the medication and therapy prescribed by them. So, the hospital staff can now focus on those in dire need.
The cost, time and resources which can be saved due to telemedicine are, therefore, a major part of the appeal.
Types of Telemedicine
- Store-and-forward: Store-and-forward telemedicine is common in the medical fields of dermatology, radiology, and pathology. All the relevant data of a patient is gathered and then transferred to a secure cloud-based platform that authorised users can access. The biggest benefit of store-and-forward telemedicine is that it allows providers to apply evidence-based care to make more accurate diagnoses and treatment recommendations.
- Remote monitoring: This type of telemedicine uses a range of technological devices to monitor the health and clinical signs of a patient with chronic diseases such as cardiovascular disease, diabetes mellitus, and asthma. Besides frequent monitoring and cost-cutting, the most significant benefit of remote patient monitoring is the independence that patients get from making regular trips to care facilities without giving up on the quality of healthcare and allows doctors to keep an eye on the patients’ progress and receive alerts if any stats indicate declining conditions.
- Real-time interactive services: Real-time, or live telemedicine, enables remote medical consultations in real-time. It uses two-way communication tools like video conferencing, live chat, or phone calls to conduct medical examinations. Each of these has a beneficial role in overall health care and, when properly utilised, can be beneficial for both healthcare providers and patients.
Rise of Telemedicine With COVID-19
With the COVID-19 outbreak causing worldwide lockdowns and the fall of conventional health systems due to the lack of either vaccines or effective treatments, telemedicine and e-health applications helped patients virtually communicate with their general practitioners and specialists.
United Kingdom’s NHS 111 approach to the coronavirus diagnosis is an example of telehealth services in action. Patients can access medical advice over the phone, with qualified call handlers advising them on everything, from self-isolating procedures to insights about coronavirus testing.
The remote diagnostic procedures have also helped doctors to optimise the use of personal protective equipment (PPE) for front-line health workers.
The COVID-19 Healthcare Coalition, in a survey of roughly 1600 healthcare providers, found that almost 70% were motivated to use more telehealth services because of the experiences they’ve had during the coronavirus pandemic.
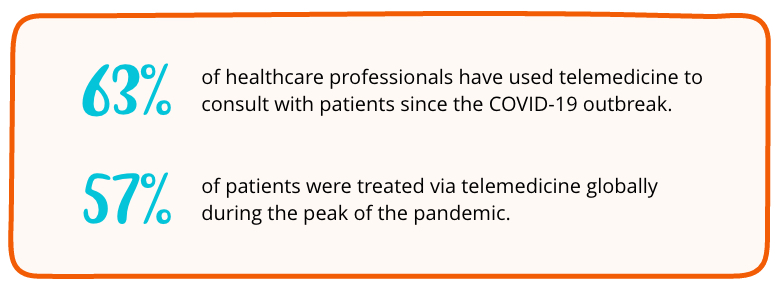
With these statistics in mind, we can safely assume that telemedicine is here to stay.
Role Of Multilingual Interpretation In Telemedicine
With more and more clinicians and patients relying on telemedicine, it might cause and deepen existing healthcare disparities, such as creating communication barriers for non-English speakers.
We are undoubtedly in an era where English is the principal language of modern medicine. While this helps maintain uniformity, patients with limited English proficiency may experience additional communication barriers to engaging with telemedicine.
Despite the attempts to provide equal access to healthcare for all, most telemedicine-specific platforms have little to no language support for patients who do not speak the national or official language of the country they reside in.
While telemedicine platforms are proving to be beneficial for many during the pandemic, a considerable fraction of the population isn’t able to participate in these virtual medicare sessions due to the lack of language services.
Most countries are home to domestic populations with more than one native language. Hence, it is crucial that patients must receive the care they need in their primary language. Furthermore, even the most skilled clinician cannot provide high-quality healthcare services to a broad and diverse audience without accurate interpretation by trained and qualified medical interpreters with a working knowledge of medical terminology and medical systems.
Interpreters can provide clear multilingual communication through telemedicine channels by interpreting and translating information for the medical staff and the patient so medical workers can adequately attend to the patient’s symptoms, concerns or questions. While we cannot forget to localise the manuals for telemedicine apps and software, the use of interpreters on the phone and video visits also needs specific attention. Moreover, optimising three-way calling and video medical interpretation is a priority for safety-net healthcare systems to launch their telehealth programs successfully.
In rural populations, telehealth interpreting offers improved care delivery to support positive health outcomes for limited-English proficient patients. Amid a global health crisis, when in-person visits aren’t always safe or viable, the right technology and an experienced interpreter with a command of a wide range of medical terminology are key to ensuring a successful telehealth session.
Language solutions such as these increase the reach of telehealth services and create meaningful customer connections.
Hiring Interpreters For Your Telemedicine Sessions
- Pre-Session or Preparatory Session: Most language service providers and even medical workers prefer to have a prep session to be clear about various things like the nature of the call, the mode of interpreting to be used, use of highly technical language and any important points to remember before meeting the patient. This provides the interpreter with the necessary information to make adjustments in his/her interpreting to make the session smoother for all three parties.
- Audio Sessions: An interpreter, medical professional, and the patient all are connected via a telephonic phone call. This is the easiest and the fastest method of telemedicine and requires no other specialised hardware.
- Video Sessions: Video remote interpretation, or VRI, provides the highest level of correctness with the added visual support of the interpreter. VRI also allows clinicians to communicate with deaf and hard-of-hearing patients.
A Checklist For Hiring A Telemedicine Interpretation Service
As a highly skilled and specialised field of work, medical interpretation should only be undertaken by qualified linguists. Besides being fluent in two or more languages, a medical interpreter must exhibit many other skills and attributes. Make sure that you spot these qualities in the Interpretation Service Provider that you select:

- HIPAA compliance: To ensure that all the sensitive medical information you share during a telemedicine interpretation session is protected, you must hire a provider which is HIPAA (Health Insurance Portability and Accountability Act) compliant.
- Empathy: When it comes to interpreting in medical situations, the linguist needs to possess the quality of compassion and must understand the heaviness of the case to modify the tone, the manner and figure out the best possible way to perform his duty.
- Cultural Awareness: The most underrated yet highly impactful quality in an interpreter is one of being aware of the patient's cultural background. This helps the interpreter choose their language carefully and brings clarity about the accent, cultural context, and a lot more.
- Professional boundaries and ethics: Medical interpreters may be involved in highly delicate and high profile cases, including fatalities and emotional trauma. In such instances, they have to show high levels of resilience and professionalism with the people they are there to interpret for.
- Expertise in the medical field: Understanding the complex medical jargons requires brilliant knowledge and experience, and a good interpreter must be well aware of these. This makes it much easier for the patient to understand what the doctors are trying in a layman’s language. In addition, they must always be open to learning new things and should have good grasping skills.
Conclusion
Telemedicine has not been used traditionally for any public health crises in the past, but that is vigorously changing with the COVID-19 flux. Medical interpretation services can help to provide telemedicine services to a larger and broader audience. Utilising qualified and professional interpreters to facilitate proper communication between patient-doctor ensures equal access to healthcare for all. In addition, it saves time, money, and resources to give us hope for a better quality of life.